In a 2010 study of nursing care in an Italian hospital, researchers found that just ‘40% of nursing activities observed were included in the nursing records’ (Marinis et al, 2010). Although this study was about nurses, not prehospital medics, it indicates the potential for missing key information in our documentation. A variety of models exist to help ensure that all the useful information is in your paperwork by the time it’s finalised & to ensure that it’s clear and concise…
Before the methods are introduced, make sure to note the following:
- There is not just one method
- Patient report forms vary across Trusts. Essential (required) criteria varies too.
- Policies regarding paperwork can be found publicly on most Trust websites and will be linked to from here if permission is gained.
- There is little freely available information regarding paramedic PCR completion in the UK. Each Trust has their own policy but those policies mainly centre around mandatory fields, not around how to structure your paperwork.
- Regardless of what you use, Gregory and Mursell’s (2010: 190) recommendations include ensuring it is ‘clear, accurate and legible [,] […] objective [and] […] first hand’. However, if your information is not first hand, they advise adding the ‘name and position’ of the person who gave you the information (2010: 190).
- What do I do if I make a mistake in my paperwork? (link coming soon)
There are 8 models of documentation for medical professionals
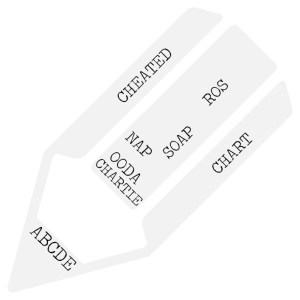
A few variations of these may exist where people have chosen to add a letter to the above acronyms to extend the models.
Doctors and websites regularly used by paramedics including Geeky Medics, seem to suggest a combination of the ABCDE, ROS & SOAP approaches, depending on the patient’s presentation (Geeky Medics, 2018).
Jump to discussion points
Jump to references
What is the ABCDE approach?

Simply, this involves transferring information from the DR ABCDE primary survey (Resuscitation Council, 2018) onto paper. Farrington (2018) mentions documenting this approach.
What is the ROS approach?

The review of systems (RoS) approach is widely used and accepted in healthcare, and easily assimilates into paramedic practice. RoS improves patient care by holistically assessing the patient, and can make the inter-professional handover of a patient to another team more professionally acceptable. Documentation using the RoS is more comprehensive and less prone to errors. (Jenkins, 2013)
ROS is:
- Also known as the systematic enquiry (Douglas et al, 2013: 35)
- Recommended by Pilbery and Lethbridge (2010: 191) and forms the structure of the secondary surveys featured in Blaber and Harris (2011).
- Part of many models of documentation & not strictly a model on its own
- Involves writing a list of systems i.e. Respiratory, Cardiovascular, Central nervous, and listing examinations beneath each subsection. So, for a patient complaining of chest pain the ROS might show:
Cardiovascular
Weak radial pulse
Tachycardic: 95.
No added heart sounds
Pitting oedema
Respiratory
Equal chest movement. No deformities to chest
Bilateral crackles on auscultation
…and so on
(The Regents of the University of California, 2015; Snadden et al, 2013)
*Note these are just examples and are not intended to demonstrate a complete patient report form.
You do not have to review every system for every patient but you should review the ones that are ‘related’ to the presenting complaint or the primary affected system (Blaber and Harris, 2011: 22).
Below is one suggested way to use ROS as part of a complete patient record form:
Presenting complaint – PC
History of Presenting Complaint – HPC
Past Medical History – PMH
Drug History – DH
Allergies
Family History – FH
Social History – SH
On Examination (O/E)
Review of Systems – ROS
Impression – IMP
Plan
(Gregory & Mursell, 2010: 191; Douglas et al, 2013: 32-39)
Variations of this model
The Douglas et al (2013: 32-39) model includes allergies in the drug history section, names review of systems as ‘systematic enquiry’, and includes the on examination section within that enquiry, rather than before it. They also add ‘information given’ to the patient and their relatives, and ‘progress notes’ to the model (Douglas et al, 2013: 39) to separate patient progress from the initial presentation & impression.
However, their model is not designed specifically for prehospital medics. Their example suggests the progress section should be used by Doctors who review patients at a later date. Gregory & Mursell’s (2010: 191) adaptation of this model is designed with Paramedics in mind. Still, a progress note section could be useful for prehospital documentation in situations where the patient’s condition changes in the relatively short time we spend with them. Following a structure which specifies documenting patient improvement or deterioration could help make our documentation clear. Comments? Add them below —>
Note, as mentioned above, that the ROS approach is part of a multitude of different approaches to writing paperwork. It is included in many of the following models either in documenting a patient’s past medical history (Beebe & Myers, 2010: 343-344) or in the secondary survey (Blaber and Harris, 2011), or both.
What is the CHART approach?

CHART stands for:
- Chief complaint
- History
- Assessment
- Rx = Drugs
- Treatment
(Beebe & Myers, 2010: 342)
What is CHARTIE?
This is the same as the above, with two additions:
- Intervention
- Evaluation
(Beebe & Myers, 2010: 342)
What is the NAP approach?

Nap stands for:
- Narrative (of the complaint)
- Assessment
- Plan of treatment
(Beebe & Myers, 2010: 342)
According to Beebe & Myers (2010), the three models listed above are now less frequently used, in favour of newer models like CHEATED.
What is CHEATED?

- Chief concern
- History
- Including the history of the complaint
- Including ‘OPQRST (onset, provocation, quality of pain, radiation, severity, timing’ (Beebe & Myers, 2010: 342) where relevant
- Including past medical history,
- Including review of systems,
- Including pertinent negatives.
- Note that Beebe & Myers (2010) recommend using the review of systems structure in order to collect information about the patient’s past medical history. Other sources, including Douglas et al (2013) use the systematic enquiry/review of systems as part of the examination section.
- Beebe & Myers (2010) include information in the history section of the CHEATED model that is more relevant for insurance-based healthcare systems. Only information relevant to UK medics has been included in this post.
- Examination of physical signs
- Assessment
- Including the patient’s consent & any refusal of care
- Treatment
- Evaluation
- ‘Following every treatment there should be an evaluation of the effectiveness of that treatment, or, at a minimum, a statement about the patient’s ongoing condition’ (Beebe & Myers, 2010: 346)
- If the patient refuses care of transport, an ‘explanation of outcomes’ can be used here (Beebe & Myers, 2010: 346).
- Disposition
- This is a summary of the patient & their treatment at the time of handover
- Worsening advice if the patient has been left at home
(Beebe & Myers, 2010: 323-346)
What is SOAP?

SOAP stands for:
- Subjective
- Patient’s feelings
- Patient’s own words
- Patient’s symptoms
- Objective
- Signs
- Clinical examination
- Assessment
- Summary of symptoms & signs
- Impression
- Plan
(Potter, 2018) – Geeky Medics
‘For the past 50 years, one of the primary organizing structures for physicians’ clinical documentation have been the SOAP note (Subjective, Objective, Assessment, Plan). The cognitive check list is well-suited to differential diagnosis but may not support detection of changes in systems and/or learning from cases.’ (Lenert, 2016)
There are several other variations of SOAP, including SNOCAMP, which adds the ‘nature of the presenting complaint, counseling, and medical decision making’ (Larimore & Jordan, 1995).
Lenert (2016) have concerns about the subjective section of the SOAP model & the potential for poor decision making due to its structure. Introducing OODA…
What is OODA?

- Observe
- Orient, including Predictions = contextualising observations, including consideration of the patient’s wishes and/or needs, prioritising, considering guidelines, consider consequences & develop plans
- Decide
- Act, including Predictions = treatment & considerations of outcomes
‘there are cognitive models that outline steps that can help novices and experienced users maintain situational awareness and learn in rapidly changing environments. One such model, which was initially developed by Boyd to help Air Force pilots outthink their opponents in aerial combat but is now widely applied within the U.S. military, is the Observe Orient Decide Act (OODA) model.’ (Lenert, 2016)
OODA is:
- Designed to be ‘a repeating loop’ (Lenert, 2016)
- ‘action-oriented’ (Lenert, 2016)
- ‘allows […] reconsideration of assumptions’ (Lenert, 2016). Put simply, it reminds us to check and re-check
- recommended in the ‘subsequent management of patients’ where SOAP is useful in the initial approach to a patient (Lenert, 2016)
‘The goal of the OODA Loop is “think” and “act” faster and better than the enemy [.] […] Bad outcomes occur when medical treatments are not adjusted fast enough, based on current hypotheses about what the illness is, to outpace progression of the illness.’ (Lenert, 2016)
It may help with ‘situational awareness, and in detecting change and errors in diagnosis.’ It may also ‘improve communications by explicitly documenting a clinician’s reasoning and decisions, much of which is not transparent in SOAP notes.’ (Lenert, 2016)
However, it’s worth bearing in mind that neither SOAP nor OODA was originally designed for pre-hospital care.
Considerations/Discussion Points
- Could OODA be used as part of a reflective framework? The model focuses on decision making and the key parts of patient assessment, which could become a reflective aid.
- Could OODA be used for time-critical patients?
- Could OODA be used as part of other models for when patients or situations become challenging or time-critical?
- E.g. a patient whose initial presentation is hypoglycaemia, who requires quick decision making but may then become stable
- e.g. a patient in an initially safe environment which later becomes unsafe & requires a new plan (for example, abusive or violent patients, relatives or bystanders, or environmental dangers)
- In these cases, OODA could be used to document & assist with decision making during parts of jobs.
- CHEATED, CHARTIE, OODA and Douglas et al’s (2013: 39) version which includes ROS all have some sort of evaluation featured as part of their models. A useful addition?
Comments? Questions? Add them below –>
References
Beebe, R. & Myers, J. 2010. Foundations of Paramedic Care, Volume 1. Delmar: Cengage Learning
Blaber, A.Y. & Harris, G. 2011. Assessment skills for paramedics, Berkshire: Open University Press
Douglas, G. et al, 2013. Macleod’s Clinical Examination, Edinburgh: Elsevier. Ed. 13.
Farrington, G. 2018. ABCDE Approach, Available Online: https://geekymedics.com/abcde-approach/ (Accessed 16/06/18)
Geeky Medics, 2018. Documentation. Available Online: https://geekymedics.com/category/communication-skills/documentation/ (Accessed 16/06/18)
Gregory, P. & Mursell, I. 2010. Manual of Clinical Paramedic Procedures, Oxford: Blackwell Publishing
Jenkins, S. 2013. History taking, assessment and documentation for paramedics. Journal of Paramedic Practice, 5 (6): 310-316
Larimore, W.L. & Jordan, E.V. 1995. SOAP to SNOCAMP: Improving the medical record format, The journal of family practice, 41 (4): 393-398
Lenert, L.A. 2016. Toward Medical Documentation That Enhances Situational Awareness Learning, AMIA Annual Symposium Proceedings Archive, 2016: 763-771
Marinis, D. et al (2010) ‘If it is not recorded, it has not been done!’? consistency between nursing records and observed nursing care in an Italian hospital. 19. (11-12). 1544-52. doi: 10.1111/j.1365-2702.2009.03012.x
Pilbery, R. & Lethbridge, K. 2016. Ambulance Care Practice, Bridgwater: Class Professional Publishing
Potter, L. 2018. How to document a patient assessment (SOAP), Available Online: https://geekymedics.com/document-patient-assessment-soap/ (Accessed 16/06/18)
Resuscitation Council, 2018. The ABCDE Approach, Available Online: https://www.resus.org.uk/resuscitation-guidelines/abcde-approach/ (Accessed 16/06/18)
Snadden, D. et al. 2013. History Taking. In Douglas, G. et al Macleod’s Clinical Examination, Edinburgh: Elsevier. Ed.13.
The Regents of the University of California, 2015. Adult Review of Systems. Available Online: https://meded.ucsd.edu/clinicalmed/ros.htm (Accessed 09/06/2018)

Discover more from Article 999: Refresh, support, advance UK public health literacy & Paramedics (and similar roles).
Subscribe to get the latest posts sent to your email.